- Research
- Open access
- Published:
Sex differences of post-Covid patients undergoing outpatient pulmonary rehabilitation
Biology of Sex Differences volume 15, Article number: 36 (2024)
Abstract
Background
Following years of pandemic severe acute respiratory syndrome coronavirus 2 infections labelled Covid-19, long lasting impairment summarized as post-Covid syndrome (PCS) challenges worldwide healthcare. Patients benefit from rehabilitation programs, but sex specific aspects of improvement remain little understood. The aim of the study was to assess whether women and men differ in response to outpatient pulmonary rehabilitation for PCS.
Methods
263 (54.4% female) patients partaking in outpatient pulmonary rehabilitation (OPR) due to PCS between March 2020 and July 2022 were included in a prospective observational cohort study. Outcomes were assessed at baseline and before discharge from OPR and included six-minute walking distance (6MWD), 1-second forced expiratory volume (FEV1), diffusion capacity for carbon monoxide, maximal inspiratory pressure (MIP), dyspnea (medical research council scale), and post-Covid functional status scale (PCFS). Sexspecific changes in outcomes following OPR were assessed by linear mixed model and presented as mean differences (MD) with 95% confidence intervals. Linear regression was applied to test whether 6MWD correlates with PCFS and the minimal clinically important difference (MCID) in 6MWD regarding an improvement of at least one point in PCFS was computed with logistic regression.
Results
Significant improvement throughout OPR was observed for all outcomes (all p < 0.0001). Despite less severe Covid-19 infections, PCFS scores remained higher in females after OPR (p = 0.004) and only 19.4% of women compared to 38.5% of men achieved remission of functional impairment. At baseline as well as after OPR, females showed higher symptom load compared to men in dyspnea (p = 0.0027) and scored lower in FEV1 (p = 0.009) and MIP (p = 0.0006) assessment. Performance in 6MWD was comparable between men and women. An increase of 35 m in 6MWD was computed as minimal clinically important difference to improve functional impairment.
Conclusion
Both subjective symptoms such as fatigue and dyspnea and objective impairment in performance in pulmonary function were more frequently observed among women. Despite improvement throughout OPR in both women and men, the sex-gap in symptom load could not be closed as women less often achieved remission from functional impairment due to PCS. Intensified treatment of these symptoms should be considered in women undergoing rehabilitation for PCS.
Plain english summary
While female sex is protective during the acute infection of Covid-19, women are at increased risk of developing post-Covid syndrome (PCS) even after only mild Covid-19 infections. Severity and frequency of symptoms such as fatigue and shortness of breath are known to be higher in women compared to men. Many different rehabilitation protocols are used for PCS, but a knowledge gap regarding sex related differences in rehabilitation success remains.
Both female and male patients with PCS undergoing outpatient pulmonary rehabilitation improved in the maximum walking distance achieved within 6 min and selfrated impairment in everyday living. Although women less frequently required inpatient treatment for acute Covid-19 infection, female patients with PCS showed higher impairment in everyday living, lower capacity of physical exercise and more frequent shortness of breath, fatigue and breathing muscle weakness. Only 19.4% of women compared to 38.5% of men achieved complete remission of impairment in everyday living. Our results show that women treated for PCS retain greater symptom burden and are at risk of unsuccessful rehabilitation, calling for more targeted treatment in female patients after Covid-19 infection.
Highlights
Six weeks of outpatient pulmonary rehabilitation successfully improved 6-minute walking distance, pulmonary function and Covid-19 related functional limitations in daily living.
Women achieved remission of functional limitations less often than men (19.4% vs. 38.5%).
Women reported more severe dyspnea and showed greater impairment of maximal inspiratory pressure and forced expiratory volume compared to men.
Introduction
The ongoing Covid-19 pandemic has led to nearly 800 million people being infected with the novel severe acute respiratory syndrome coronavirus 2 (SARS CoV-2) labelled Covid-19 (https://covid19.who.int/, as of March 17th, 2024). Many patients suffer from symptoms impeding daily living longer than three months after recovery from acute infection and the term post-Covid syndrome (PCS) was established to describe this post-viral condition [1]. Recent population-based studies [2] and pooled estimates from available research [3] suggested that at least 6.5% but up to 28% of patients with Covid-19 are facing PCS, translating to 40 to 150 million cases worldwide. A recent study accounting for symptoms that were already present before Covid-19 while controlling for similar symptoms reported by patients without Covid-19 confirmed that one in eight patients with Covid-19 suffer from PCS [4]. Fatigue, dyspnea, cognitive impairment and mood or anxiety symptoms were reported by about one-third to one-half of PCS patients [2,3,4]. While clinical presentation resembles post-viral syndromes that frequently followed previous coronavirus outbreaks, i.e., SARS and Middle East respiratory syndrome [5], the scale of affected people is unprecedented. Early longitudinal studies reported a mean duration of PCS between 4 and 9 months. However, in approximately 15% of PCS cases, symptoms persisted for at least one year after testing positive for Covid-19 [3].
Sex differences impact both Covid-19 and PCS [6]. Mainly due to biological factors such as higher angiotensin convertible enzyme 2 (ACE2) mediated by sex hormones but also due to more frequent preexisting cardiovascular comorbidities men have higher rates of hospitalization and mortality in the acute infection [7], while women present more frequently with PCS and report more often core symptoms such as of dyspnea and fatigue [8]. As a result, risk factors for acute Covid-19 severity such as older age and cardiovascular comorbidities have not proven useful for assessment of PCS risk. A meta-analysis confirmed female sex among the most impactful risk factors for PCS, that more frequently develops from mild Covid-19 and at younger ages in women compared to men [9]. Next to biological differences such as X-chromosome linked immunoreactivity and protective effects of sex hormones regarding initial symptom severity, gender variables may account for higher symptom persistence in women [10]. While sex differences in symptom prevalence are well-established [4], implications for treatment of PCS and functional outcomes are scarce. The need for standardized and early interventions for PCS patients is clearly recognized. However, an abundance of rehabilitation protocols are currently deployed [11]. Here, we follow up and expand in terms of sex differences on recently reported improvement in pulmonary symptoms, exercise capacity and functional outcomes after six weeks of outpatient pulmonary rehabilitation (OPR) targeted at PCS patients [12].
Methods
Sample
The sample consists of all patients treated for PCS following a PCR-positive Covid-19 infection between March 2020 and July 2022 at the rehabilitation center ThermeWienMed (https://www.thermewienmed.at). As recently described in detail [12], all patients received six weeks of OPR following respective Austrian guidelines [13]. In short, patients completed a total of 60 rehabilitation sessions (á 50 min) split over six weeks that included a net worth of 38 h of physical exercise including endurance, strength and inspiratory muscle training in addition to diagnostic appointments, and clinical-psychological and nutritional counseling.
Baseline characteristics
At admission, next to age, sex and body mass index (BMI), presence or absence of diabetes mellitus (DM) type 1 and type 2, obesity, hyperlipidemia, arterial hypertension, diastolic dysfunction, coronary artery disease (CAD), hyperuricemia, asthma and depression (ICD-10: F32 or F33) were assessed. Severity of Covid-19 was coded mild or moderate if no inpatient treatment was required, severe if patients were admitted to hospital, and critical if patients needed intensive care. PCS symptoms were grouped into neurocognitive, musculoskeletal, gastrointestinal, cardiac and hematological symptoms, dyspnea, fatigue, autonomous dysregulation (assessed by Schellong test), lung residuals after Covid-19 (assessed by lung imaging), breathing muscle weakness (maximal inspiratory pressure (MIP) scoring below 60 and 70 mBar respectively for women and men) and diffusion impairment (assessed by diffusion capacity for carbon monoxide (DLCO) below 80% of predicted values).
Outcome variables
Expert-measured outcomes included the six-minute walking distance (6MWD) [14], 1-second forced expiratory volume (FEV1), MIP and DLCO [15]. Patient reported outcome variables included the post-Covid functional status scale (PCFS) [16], ranging from 0 (no limitations) to 3 (unable to perform usual activities) in this outpatient sample. The PCFS is the currently most established patient-rated scale for functional impairment in PCS and has been validated as useful tool for measuring PCS-related reduced quality of life. It was specifically recommended for evaluation of rehabilitation [17, 18]. Further, the modified medical research council scale (mMRC) was used for dyspnea assessment. Outcomes were assessed both as absolute values and percentages of age- and sex-adjusted reference values (%pred). Further, percentages of patients scoring below 80% of predicted reference values are reported for each outcome variable.
Statistics
Baseline characteristics were described by means and standard deviations (SD) for metric parameters and by counts and frequencies for factorial variables and tested for significance respectively by t- and chisquare tests. For PCS symptoms and comorbidities odds ratios (OR) and 95% confidence intervals (CI) were computed.
Longitudinal changes are presented descriptively both as raw values, such as 6MWD in meters, and in %pred. Mean differences (MD) are reported with 95% CI. Linear mixed effects models were computed as provided by the R package “lmer”. For each outcome variable, models were built with sex and severity of Covid-19 (dichotomized to inpatient vs. outpatient treatment) as between-subject variables and time-point (admission and discharge) as within- subject variable. Three-way interactions were computed, and patient identifier was included as random effect. In presence of significant interactions with sex, post-hoc linear mixed models were computed respectively in female and male patients with main effects of time-point and Covid-19 severity.
To assess the association between patient-reported (PCFS) and expert-measured (6MWD) primary outcomes, a generalized linear model was computed with change in PCFS in points as outcome variable and change in 6MWD in meters as predictor, adjusted for Covid-19 severity and sex. Post-hoc, Spearman correlations between change in PCFS and 6MWD were computed, stratified by significant covariates. The minimal clinically important difference (MCID) regarding 6MWD change in meters as predictor of successful reduction in PCFS by at least 1 point was assessed by the anchor method and with receiver operating characteristic curves built by univariate logistic regression.
Considering that post-Covid syndrome is a new phenomenon with high clinical urgency, all analyses were regarded as exploratory and a p-threshold of 0.05 was accepted for significance.
Results
A total of 263 patients (142 female, 54.4%) treated for respiratory symptoms or functional limitations after confirmed Covid-19 infection in the OPR center between March 2020 and July 2022 were included for analysis and are detailed in Table 1. The average time between positive testing for Covid-19 and admission to OPR was 6.5 (± 4.3) and 5.6 (± 3.6) months respectively for female and male patients (p > 0.05). Women were on average five years younger (45.0 ± 12.4 vs. 50.2 ± 12.6 years, t = -4.8, p < 0.0001) and less likely to have been hospitalized for treatment of Covid-19 (14.1% vs. 42.1%, x2 = 24.7, p < 0.0001).
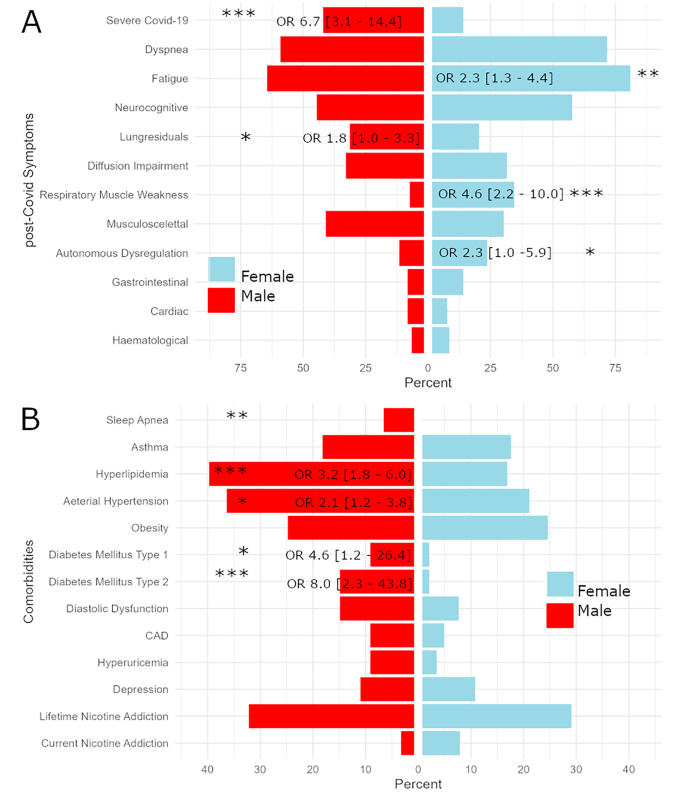
Women presented more often with dyspnea (mMRC score ≥ 2 in 37.3% vs. 21.7%, x2 = 7.9, p = 0.005), fatigue (81.0% vs. 64.5%, x2 = 8.30 p = 0.004), autonomous dysregulation (23.7% vs. 11.6%, x2 = 4.0, p = 0.047) and respiratory muscle weakness (35.3% vs. 7.4%, x2 = 27.0, p < 0.0001), while lung residuals were more often observed in men (31.4% vs. 20.4%, x2 = 3.6, p = 0.047). This pattern was observed both among patients hospitalized during acute Covid-19 infection and milder cases, detailed in Supplementary Table 1.
Regarding comorbidities, men were more often affected by DM type 1 (9.1% vs. 2.1%, x2 = 5.0, p = 0.025) and DM type 2 (14.9% vs. 2.1%, x2 = 12.8, p = 0.0003), arterial hypertension (36.4% vs. 21.1%, x2 = 6.8, p = 0.009), hyperlipidemia (39.7% vs. 16.9%, x2 = 15.9, p = 0.0001) and obstructive sleep apnea (6.6% vs. 0%, Fisher test: p = 0.018), while BMI, presence of obesity and major depressive disorder did not differ between men and women. Please also refer to Fig. 1 for sex-related OR with CI for baseline characteristics.
Bar chart opposing frequencies of post-Covid symptoms (panel A) and comorbidities (panel B) observed in female patients to that in males. Whenever significant differences in males and females were computed, odds ratios (OR) and 95% confidence intervals (CI) are presented. Significance levels are indicated by * corresponding to p < 0.05, ** to p < 0.005 and *** to p < 0.0005. Abbreviations: CAD = coronary artery disease
6MWD
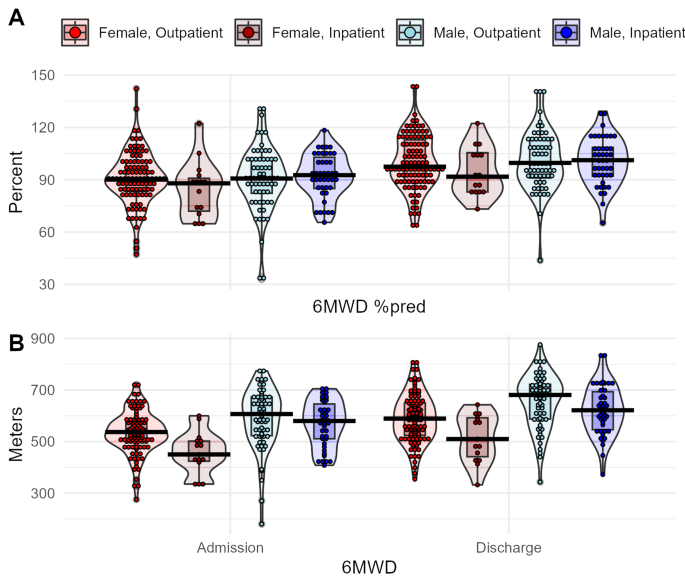
On average, at admission women walked 525.2 m (± 85.5) and men walked 581.9 m (± 106.25) of 6MWD. Before OPR, women scored 8.5%-points (CI 0.7–16.3) lower in 6MWD%pred, and 24.6% of women compared to 19.8% of men ranked below 80% of 6MWD%pred. Patients improved over time (F1, 218 = 238.6, p < 0.0001), while no main or interaction effects of sex or Covid-19 severity were observed. At discharge from OPR, the MD in 6MWD%pred between females and males was 5.6%-points (CI 2.5–13.8) and 10.2% of women compared to 3.8% of men still scored below 80% of their predicted reference values. Please also refer to Fig. 2 for violin plots depicting performance in 6MWD. A complete list of mixed model results is provided in Table 2.
Boxplot diagrams of physical performance assessed by 6-minute walking distance (6MWD). Colors indicate sample stratification by sex and severity of Covid-19. Panel A shows the ratio between achieved distance and predicted values based on age- and sex-adjusted reference equations, panel B raw values in meters walked
Pulmonary outcomes
Interactions effects between sex and respectively time-point (F1, 227 = 3.9, p = 0.051) and Covid-19 severity (F1, 227 =6.9, p = 0.009) were computed for FEV1%pred. Despite the lack of a significant threeway interaction, sex differences in improvement were observed mostly in patients with severe Covid-19 infection that showed a MD between time-points of 124%points in men compared to 0.2%-points in women. Regarding DLCO, improvement over time (F1, 181 = 16.2, p = 0.0001) but no main or interaction effects of sex were observed.
A significant interaction between sex and time-point was computed for MIP%pred (F1, 225 = 5.9, p = 0.016). MIP%pred was decreased in women compared to men by a MD of 16.5%-points (CI 9.3–23.6) at admission. Despite stronger relative improvement in females shown by average change between time-points of 31.5%-points (CI 24.2–38.8) compared to 23.9%-points (CI 16.5–31.4) in men, women still scored lower MIP%pred compared to men at discharge by a MD of 8.9%-points (CI 1.3–16.6). Inspiratory muscle weakness was present in 34.5% of women but only 7.4% of men at baseline. After rehabilitation, 9.2% of women and a single man still fulfilled criteria for inspiratory muscle weakness.
Women reported more dyspnea on the mMRC scale (F1, 237 = 9.2, p = 0.003) compared to men, both at admission (MD 0.3, CI 0.1–0.5) and after rehabilitation (MD 0.2, CI 0.04–0.4). Further, an interaction effect on mMRC score between Covid-19 infection severity and sex was found (F1, 237 = 2.9, p = 0.051). Only among women, severe Covid-19 was linked to higher mMRC scores (F1, 132 = 11.0, p = 0.001). Please also refer to Supplementary Figs. 3–5 for violin plots depicting pulmonary outcomes.
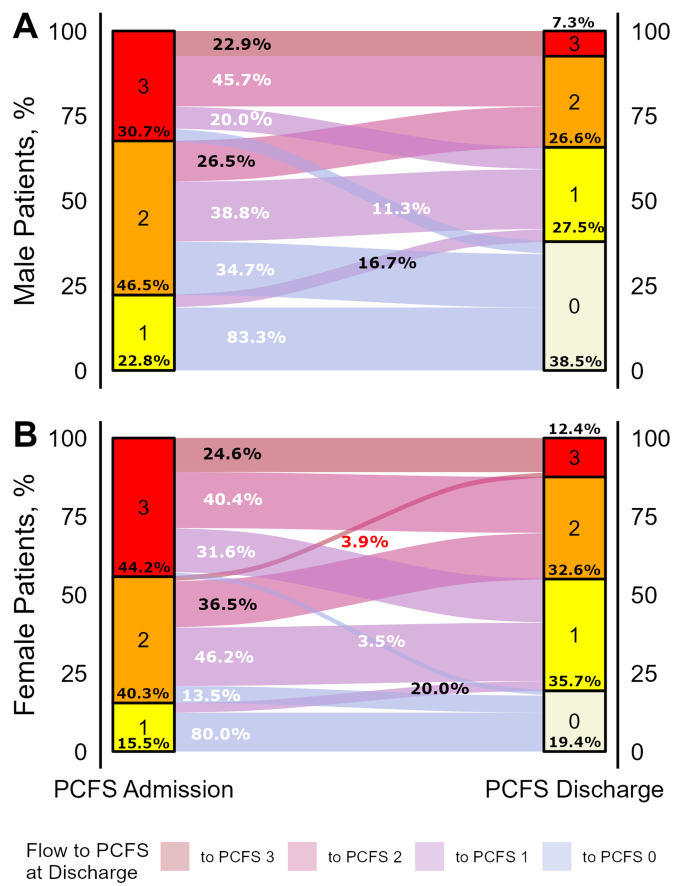
PCFS scale
At admission to OPR, 85.2% of female and 77.2% of male patients reported a PCFS score ≥ 2 indicating clinically relevant functional limitations. An increase of at least one point in PCFS was achieved by 68.5% of female compared to 74.5% of male patients. Despite improvement in PCFS over time both in women and men (F1, 234 = 295.8, p < 0.0001), female patients showed more severe limitations in daily living compared to men (F1, 234 = 8.3, p = 0.004). At admission, 44.2% of women scored PCFS of 3 compared to 30.7% of men. At discharge, clinically relevant impairment indicated by PCFS score ≥ 2 was still reported by 45.0% women compared to 33.9% of men. Remission (PCFS of 0) was also achieved by fewer women (19.4%) than men (38.5%).
In summary, 60.1% of patients reported PCFS ≤ 1 after OPR and thus benefitted from rehabilitation. A quarter of the remaining 39.9% of patients in need of further rehabilitation can be considered non-responders to OPR as they still scored PCFS of 3 at discharge. Only two patients worsened in PCFS over the course of OPR, both of which were women. Please refer to Fig. 3 for an alluvial plot detailing changes in PCFS scores respectively for women and men.
Flow diagram showing changes in post-Covid functional status (PCFS) scale between admission and discharge from pulmonary outpatient rehabilitation. Flow trajectories are sized according to the patient numbers following them and colors indicate the PCFS score at discharge. Numbers indicate percentages of patients flowing from each stratum of PCFS score at admission, respectively colored white for patients that achieve a drop of at least one point in PCSF score, black for patients with stagnant PSCFS score, and red for patients with worsened PCFS scores at discharge. Example given, 3.5% of female patients compared to 11.3% of male patients with a PCFS score of 3 at admission achieved full remission indicated by a PCSF score of 0
Absolute change in PCFS was associated with the interaction between absolute change in 6MWD in meters and severity of Covid-19 (F = 5.4, p = 0.021). The association between changes in 6MWD and PCFS was only present in those treated as inpatients for severe Covid-19 infection (F = 10.3, p = 0.002). Changes in PCFS and 6MWD showed a moderate Spearman correlation in patients who had severe (r = 0.41, p = 0.003) but not in those with mild to moderate (r = 0.07, p > 0.05) Covid-19 infection (Supplementary Fig. 1). An improvement of 35 m in 6MWD was identified as MCID, corresponding to an increase of at least one point in PCFS, and was achieved by 61.5% of women and 63.8% of men. A sensitivity of 72.5% and specificity of 53.5% was achieved to classify patients with and without improvement of PCFS (Supplementary Fig. 2). In the subsample of patients with severe Covid-19 infection, the same cut-off of 35 m allowed better performance with a sensitivity 77.8% and specificity of 75%.
Discussion
In consecutive patients with PCS undergoing six weeks of OPR, significant improvement was observed in exercise capacity and respiratory function. These results reinforce our previous report on the success of OPR in a preliminary sample of 64 patients [12], while emphasizing the importance of sex differences in PCS symptom presentation and outcome. Women showed worse functioning in daily activities measured by PCFS. Rehabilitation failed to bridge the gap separating them from men regarding PCFS scores, symptom burden of dyspnea, and objectified performance in MIP.
The rate of hospitalization during the acute Covid-19 infection was considerably lower among women (14.1%) compared to men (42.1%), which is in line with higher morbidity and mortality in men during acute Covid-19 infection demonstrated in prior studies [7]. These sex-gaps were attributed to biological differences in women and men such as higher ACE2 in men that is used by SARS-CoV-2 for cell entry [19]. Thereby, male sex hormones testosterone and dihydrotestosterone were suggested to upregulate ACE2, suppress immune responses and increase endothelial damage in Covid-19. Prolonged hospitalization and admission are known to bring along cardiorespiratory sequelae and a need for rehabilitation, suggesting higher need of OPR in men following Covid-19. However, in this cohort of patients with PCS undergoing OPR both physical and functional limitations were significantly higher in women despite having suffered predominantly mild acute infections of Covid-19. Our results agree with consistent observations that women develop Covid-19 more often than men following mild infections and that initial severity is of limited prognostic value for PCS [20]. Importantly, women did not only endorse more subjective symptoms such as fatigue and dyspnea as previously reported [20,21,22] but also showed higher rates of objective pulmonary impairment such as decreased inspiratory muscle strength throughout OPR.
The reasons for observed sex differences are less understood in PCS compared to acute Covid-19 infections. Fatigue is a central symptom of affective disorders such as depression as well as syndromes associated with exposure to viral infections known prior to Covid-19 such as myalgic-encephalomyelitis/chronic-fatigue-syndrome (ME/CFS) [23, 24]. A sex-gap with female overrepresentation is well-documented in both depression and ME/CFS and is putatively owed to both gender-related variables and biological factors. Conversely to acute virus infections that more severely affect men, women may be disadvantaged regarding post-viral syndromes such as ME/CFS and PCS by prolonged immune responses that lead to endothelial dysfunction [19]. Further, sex differences regarding responses of the hypothalamic-pituitary-adrenal (HPA) axis to acute and chronic stress are well-established and enhanced activity in women was suggested as contributing factor to higher rates of stress-related disorders such as depression [25]. Direct impairment of the pituitary gland and HPA dysregulation may occur during Covid-19 and cause typical symptoms of PCS such as fatigue in sex-dependent manner [26].
Furthermore, sex hormones and particularly low estrogen were previously associated with depression and ME/CFS and may also be relevant to PCS considering that symptoms such as fatigue and low mood are shared with menopause [27]. Interestingly, most pronounced sex differences in PCS symptom presentation were observed in patients below 50 years of age in a cohort followed-up after hospitalization due to Covid-19. Here, the average age of women was 45 years which suggest perimenopausal states in a relevant portion of female patients. Disruptions of the female menstrual cycle with transient disturbance of sexual hormones were observed inconsistently in PCS and may in part be responsible for symptoms predominantly seen in women with PCS [24].
Besides biological sex, gender roles typically assumed by women also contribute to clinical differences observed in PCS. Gender perspectives on Covid-19 were rarely considered despite early calls for implementation reflecting on the foreseeably disproportionate impact of the pandemic on female and male working- and social-life [28]. Particularly in non-hospitalized patients with Covid-19, female gender measured by a composite score was a stronger predictor for PCS than biological sex [20]. Living alone was a strong predictor for PCS in women but a protective factor in men, indicating interplay of socioeconomic and psychosocial factors. The role of gender in rehabilitation is still unknown and calls for further research.
Along these lines, psychiatric comorbidities preexisting Covid-19 infection more frequently in women than men due to gender and sex-related risk factors may explain differences in PCS presentation. While rates of depression documented prior to admission were comparable between women (10.6%) and men (10.7%) in this sample, higher rates of psychiatric comorbidities in women with PCS was recently reported by a large epidemiological sample [20]. Both in treatment of depression and rehabilitation, fatigue is known to be an unfavorable prognostic marker [29]. The higher rates of fatigue observed in women at baseline may therefore indicate a higher load of newly onset or aggravated neuropsychiatric symptoms that require specialized treatments.
Regarding functional limitations, the PCFS scale was designed to comprehensively rate impairment in daily activities in PCS patients and was applied in a broad spectrum of studies [16,17,18]. At admission, on average 6 months after Covid-19 infection, 44.2% of female compared to 30.7% of male patients reported severe impairment (PCFS of 3). As changes in PCFS were similar in women and men, higher impairment in women was still observed after completing rehabilitation. Stratification by baseline functional limitations revealed similar trajectories for men and women presenting with mild impairment (PCFS of 1), showing remission in 83% and 80% of cases. However, respectively with moderate (PCFS 2) and severe (PCFS 3) limitations at admission, 34.7% and 11.4% of men showed complete remission, compared with 13.5% and 3.5% of women. On the other hand, a stagnant PCFS score indicating resistance to rehabilitation was seen in 30.2% of women and 22.9% of men. In summary, more than a third of male patients (38.5%) achieved complete remission of functional impairment (PCFS of 0), compared to less than a fifth of female patients (18.9%).
Despite reporting more functional impairment, women did not underperform regarding 6MWD. Scores below 80% of 6MWD%pred, commonly used as threshold of norm values, were seen in 22.8% of patients at admission to rehabilitation. Roughly three-quarters of these clinically impaired patients successfully improved their walking distance to norm ranges until discharge. These numbers as well as absolute 6MWD are in line with findings in 83 Chinese patients followed up three and six months after inpatient treatment for severe Covid-19 in Wuhan [30], but diverge from reports of PCS patients with substantially lower 6MWD of 461 m [31], and cohorts with up to half of patients scoring 6MWD below 80% [32]. Females may thereby be at increased risk for scoring below the norm threshold [33]. On the other hand, an Italian study stratifying 75 PCS patients by Covid-19 symptom load reported mostly unimpaired 6MWD, even in the severe symptoms group [34]. Another study comparing PCS patients to Covid-19 negative patients matched by sex, age and cardiovascular profile also observed similar performance in 6MWD [35]. A comprehensive study on all confirmed cases with desaturated oxygen below 94% in Iceland drew a more distinct picture with lowered 6MWD observed only in patients treated in intensive care during Covid-19 [36]. This finding was supported by a study comparing intensive care to other hospitalized patients [37]. This distinction is also observed in the present study. Compared to outpatients and non-intensive-care inpatients, especially female (22.7% in non-intensive care vs. 66.6% in intensive care) but also male (18.2% vs. 29.4%) patients that had been admitted to intensive care units showed considerably higher rates of impaired 6MWD. Regardless of these considerations, rehabilitation programs targeting PCS were demonstrated to successfully raise 6MWD [12, 38,39,40]. Patients undergoing three weeks of cardiopulmonary rehabilitation in Poland improved on average 42.5 m, a comparable finding to the 55 and 61 m observed here respectively for women and men after six weeks [39]. However, the clinical importance of 6MWD as a marker for functional outcome in PCS can be questioned considering both that a significant portion of PCS patients show 6MWD within the normal ranges and that especially women often remain clearly impaired despite achieving an improvement of 35 m or more deemed clinically relevant. Change in 6MWD showed moderate correlation with change in PCFS score in patients with severe but poor correlation in patients with mild to moderate Covid-19 infection. Hence, we argue that 6MWD does not provide a complete picture of rehabilitation success and likely reflects subjective improvement only in patients that were hospitalized for treatment of their Covid-19 infection.
Pronounced sex differences were observed in respiratory muscle strength assessed by MIP. that are in line with previous reports of impairment in women with PCS [41]. Scores in MIP below the established ranges of 60 mbar for women and 70 mbar for men were observed in 35.4% of females but only 7.4% of males. Despite relatively stronger improvement in females, still 9.2% of women compared to a marginal 0.8% of men remained in the clinically relevant low range. Regarding FEV1, considerably worse scores in patients with severe Covid-19 were observed. Interestingly, male patients with severe Covid-19 successfully closed the gap in FEV1 separating them from those with mild Covid-19 during OPR, while female patients did not. Regarding subjective pulmonary symptoms, women reported higher mMRC scores throughout the observation period. Female sex was previously linked to pulmonary symptoms [30, 41]. Here, roughly 80% of patients that presented moderate to severe dyspnea at admission successfully improved over the course of OPR. However, only 47.2% of women compared to 64.5% of men showed complete remission of dyspnea, potentially due to higher rates of impaired inspiratory muscle strength in women. In synopsis, OPR was effective in improving pulmonary outcomes especially in patients with higher impairment, i.e., females regarding MIP and patients with severe Covid-19 regarding FEV1. Nevertheless, more severe residual impairment in women calls for targeted interventions.
Reflecting on these results, selection bias must be considered as the most important limitation. Considerable differences in baseline symptoms across rehabilitation services indicate ambiguity in patient allocation [40], although the pattern of sex-differences resembles well-replicated findings of PCS more often manifesting in women following mild infections [20]. Despite controlling for the severity of the acute Covid-19 infection, we cannot fully rule out that differences in OPR outcomes were driven by earlier phases of the infection. Further, only patients eligible for outpatient rehabilitation were included in this analysis and thus different patterns may be observed in inpatient rehabilitation. Some studies have suggested that sex-differences to be less pronounced in hospitalized and elderly patients potentially due a stronger role of cardiovascular comorbidities that cross out some of the sex- and gender-related effects demonstrated in PCS [20]. Consequently, we cannot generalize the findings presented here to other cohorts of PCS patients.
Furthermore, other follow-up studies at various time points after Covid-19 observed improvement of physical performance and to some extent of typical PCS symptoms as a function of time rather than rehabilitation [30]. While controlled trials are exceedingly rare, a study matching confirmed Covid-19 cases to patients without Covid-19 but similar other risk factors observed no differences in standard assessments such as 6MWD [35]. Hence, we cannot verify that the observed improvement was in fact caused by the rehabilitation program alone.
Further, reference equations that are commonly applied to resolve physiological sex- and age-related differences in performance were shown to lack congruency and are dependent on their data-context [42]. Finally, we cannot rule out false positive results due broad application of tests in an explorative manner.
Perspectives and significance
OPR is demonstrated to be an effective and safe measure to facilitate subjective as well as objective recovery from PCS symptoms and impairment in daily activities. However, sex differences in PCS rehabilitation outcomes hold important implications for clinical practice. Women present more often with highly prevalent PCS symptoms fatigue and dyspnea and are more severely limited by these symptoms in daily living. Here we show that women and men show improvement during rehabilitation in all recorded outcomes, while underlining that more targeted protocols are called for to enable women to bridge the gap still separating them from more favorable outcomes observed in men at rehabilitation discharge. These may include earlier as well as modular interventions addressing sex differences in functional status and specific symptom presentations such as dyspnea and breathing muscle weakness.
Data availability
Data are available from the corresponding author on reasonable request.
References
Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27(4):601–15.
Peter RS, Nieters A, Krausslich HG, Brockmann SO, Gopel S, Kindle G, et al. Post-acute sequelae of covid-19 six to 12 months after infection: population based study. BMJ. 2022;379:e071050.
Global Burden of Disease Long CC, Wulf Hanson S, Abbafati C, Aerts JG, Al-Aly Z, Ashbaugh C, et al. Estimated global proportions of individuals with persistent fatigue, cognitive, and respiratory symptom clusters following symptomatic COVID-19 in 2020 and 2021. JAMA. 2022;328(16):1604–15.
Ballering AV, van Zon SKR, Olde Hartman TC, Rosmalen JGM, Lifelines Corona Research I. Persistence of somatic symptoms after COVID-19 in the Netherlands: an observational cohort study. Lancet. 2022;400(10350):452–61.
Ahmed H, Patel K, Greenwood DC, Halpin S, Lewthwaite P, Salawu A, et al. Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: a systematic review and meta-analysis. J Rehabil Med. 2020;52(5):jrm00063.
Haque A, Pant AB. Long covid: untangling the Complex Syndrome and the search for therapeutics. Viruses. 2022;15(42).
Gebhard CE, Hamouda N, Gebert P, Regitz-Zagrosek V, Gebhard C, Investigators C. Sex versus gender-related characteristics: which predicts clinical outcomes of acute COVID-19? Intensive Care Med. 2022;48(11):1652–5.
Pela G, Goldoni M, Solinas E, Cavalli C, Tagliaferri S, Ranzieri S, et al. Sex-related differences in Long-COVID-19 syndrome. J Womens Health (Larchmt). 2022;31(5):620–30.
Maglietta G, Diodati F, Puntoni M, Lazzarelli S, Marcomini B, Patrizi L et al. Prognostic factors for Post-COVID-19 syndrome: a systematic review and Meta-analysis. J Clin Med. 2022;11(6).
Gebhard CE, Sütsch C, Bengs S, Deforth M, Buehler KP, Hamouda N, et al. Sex- and gender-specific risk factors of Post-COVID-19 syndrome: a Population-based Cohort Study in Switzerland. medRxiv. 2021. 2021.06.30.21259757.
Decary S, De Groote W, Arienti C, Kiekens C, Boldrini P, Lazzarini SG, et al. Scoping review of rehabilitation care models for post COVID-19 condition. Bull World Health Organ. 2022;100(11):676–88.
Nopp S, Moik F, Klok FA, Gattinger D, Petrovic M, Vonbank K, et al. Outpatient Pulmonary Rehabilitation in patients with long COVID improves Exercise Capacity, Functional Status, Dyspnea, fatigue, and Quality of Life. Respiration. 2022;101(6):593–601.
Vonbank K, Zwick RH, Strauss M, Lichtenschopf A, Puelacher C, Budnowski A, et al. [Guidelines for outpatient pulmonary rehabilitation in Austria]. Wien Klin Wochenschr. 2015;127(13–14):503–13.
Enright PL, Sherrill DL. Reference equations for the six-minute walk in healthy adults. Am J Respir Crit Care Med. 1998;158(5 Pt 1):1384–7.
Evans JA, Whitelaw WA. The assessment of maximal respiratory mouth pressures in adults. Respir Care. 2009;54(10):1348–59.
Klok FA, Boon G, Barco S, Endres M, Geelhoed JJM, Knauss S et al. The Post-COVID-19 functional status scale: a tool to measure functional status over time after COVID-19. Eur Respir J. 2020;56(1).
Machado FVC, Meys R, Delbressine JM, Vaes AW, Goertz YMJ, van Herck M, et al. Construct validity of the Post-COVID-19 functional status scale in adult subjects with COVID-19. Health Qual Life Outcomes. 2021;19(1):40.
Benkalfate N, Eschapasse E, Georges T, Leblanc C, Dirou S, Melscoet L et al. Evaluation of the Post-COVID-19 functional status (PCFS) scale in a cohort of patients recovering from hypoxemic SARS-CoV-2 pneumonia. BMJ Open Respir Res. 2022;9(1).
Kitselman AK, Bedard-Matteau J, Rousseau S, Tabrizchi R, Daneshtalab N. Sex differences in vascular endothelial function related to acute and long COVID-19. Vascul Pharmacol. 2023;154:107250.
Gebhard CE, Sutsch C, Gebert P, Gysi B, Bengs S, Todorov A et al. Impact of sex and gender on post-COVID-19 syndrome, Switzerland, 2020. Euro Surveill. 2024;29(2).
Nasserie T, Hittle M, Goodman SN. Assessment of the frequency and Variety of persistent symptoms among patients with COVID-19: a systematic review. JAMA Netw Open. 2021;4(5):e2111417.
Sigfrid L, Drake TM, Pauley E, Jesudason EC, Olliaro P, Lim WS, et al. Long covid in adults discharged from UK hospitals after Covid-19: a prospective, multicentre cohort study using the ISARIC WHO Clinical Characterisation Protocol. Lancet Reg Health Eur. 2021;8:100186.
Malgaroli M, Calderon A, Bonanno GA. Networks of major depressive disorder: a systematic review. Clin Psychol Rev. 2021;85:102000.
Pollack B, von Saltza E, McCorkell L, Santos L, Hultman A, Cohen AK, et al. Female reproductive health impacts of long COVID and associated illnesses including ME/CFS, POTS, and connective tissue disorders: a literature review. Front Rehabil Sci. 2023;4:1122673.
Heck AL, Handa RJ. Sex differences in the hypothalamic-pituitary-adrenal axis’ response to stress: an important role for gonadal hormones. Neuropsychopharmacology. 2019;44(1):45–58.
Taieb A, Nassim BHS, Asma G, Jabeur M, Ghada S, Asma BA. The growing understanding of the Pituitary implication in the pathogenesis of long COVID-19 syndrome: a narrative review. Adv Respir Med. 2024;92(1):96–109.
Stewart S, Newson L, Briggs TA, Grammatopoulos D, Young L, Gill P. Long COVID risk - a signal to address sex hormones and women’s health. Lancet Reg Health Eur. 2021;11:100242.
Wenham C, Smith J, Morgan R, Gender, Group C-W. COVID-19: the gendered impacts of the outbreak. Lancet. 2020;395(10227):846–8.
Fava M, Ball S, Nelson JC, Sparks J, Konechnik T, Classi P, et al. Clinical relevance of fatigue as a residual symptom in major depressive disorder. Depress Anxiety. 2014;31(3):250–7.
Wu X, Liu X, Zhou Y, Yu H, Li R, Zhan Q, et al. 3-month, 6-month, 9-month, and 12-month respiratory outcomes in patients following COVID-19-related hospitalisation: a prospective study. Lancet Respir Med. 2021;9(7):747–54.
Peroy-Badal R, Sevillano-Castano A, Torres-Castro R, Garcia-Fernandez P, Mate-Munoz JL, Dumitrana C et al. Comparison of different field tests to assess the physical capacity of post-COVID-19 patients. Pulmonology. 2022.
Aranda J, Oriol I, Feria L, Abelenda G, Rombauts A, Simonetti AF, et al. Persistent COVID-19 symptoms 1 year after hospital discharge: a prospective multicenter study. PLoS ONE. 2022;17(10):e0275615.
Spicuzza L, Campisi R, Alia S, Prestifilippo S, Giuffrida ML, Angileri L et al. Female sex affects respiratory function and Exercise ability in patients recovered from COVID-19 Pneumonia. J Womens Health (Larchmt). 2022.
Ora J, Zerillo B, De Marco P, Manzetti GM, De Guido I, Calzetta L, et al. Effects of SARS-CoV-2 infection on pulmonary function tests and Exercise Tolerance. J Clin Med. 2022;11:17.
Haberland E, Haberland J, Richter S, Schmid M, Hromek J, Zimmermann H, et al. Seven months after mild COVID-19: a single-centre controlled Follow-Up study in the District of Constance (FSC19-KN). Int J Clin Pract. 2022;2022:8373697.
Axelsson GT, Halldorsson AB, Jonsson HM, Eythorsson E, Sigurdardottir SE, Hardardottir H et al. Respiratory function and CT abnormalities among survivors of COVID-19 pneumonia: a nationwide follow-up study. BMJ Open Respir Res. 2022;9(1).
Pini L, Montori R, Giordani J, Guerini M, Orzes N, Ciarfaglia M et al. Assessment of respiratory function and exercise tolerance at 4–6 months after COVID-19 infection in patients with pneumonia of different severity. Intern Med J. 2022.
Hasenoehrl T, Palma S, Huber DF, Kastl S, Steiner M, Jordakieva G et al. Post-COVID: effects of physical exercise on functional status and work ability in health care personnel. Disabil Rehabil. 2022:1–7.
Loboda D, Gibinski M, Wilczek J, Paradowska-Nowakowska E, Ekiert K, Rybicka E et al. Effectiveness of cardiopulmonary rehabilitation after COVID-19 in Poland. Pol Arch Intern Med. 2022.
Berentschot JC, Heijenbrok-Kal MH, Bek LM, Huijts SM, van Bommel J, van Genderen ME, et al. Physical recovery across care pathways up to 12 months after hospitalization for COVID-19: a multicenter prospective cohort study (CO-FLOW). Lancet Reg Health Eur. 2022;22:100485.
Prestes GDS, Simon CS, Walz R, Ritter C, Dal-Pizzol F. Respiratory outcomes after 6 months of Hospital Discharge in patients affected by COVID-19: a prospective cohort. Front Med (Lausanne). 2022;9:795074.
Zou H, Zhu X, Zhang J, Wang Y, Wu X, Liu F, et al. Reference equations for the six-minute walk distance in the healthy Chinese population aged 18–59 years. PLoS ONE. 2017;12(9):e0184669.
Funding
The research was supported by a grant of the Austrian “Medizinisch-wissenschaftlicher Fonds des Bürgermeisters der Bundeshauptstadt Wien“ awarded to S. Nopp (Nr. 21224).
Author information
Authors and Affiliations
Contributions
A.K. was responsible for data management, statistics and preparation of the manuscript. S.N. was involved in planning and implementation of the study rationale, data presentation and preparation of the manuscript. D.G. and M.P. were involved in collection of clinical data and management of patient related tasks. M.A. and D.S. were involved in data management and preparation of the manuscript. A.K.-W. was advising on study planning, advising study methods and assisting preparation of the manuscript. R.Z. was leading study planning, supervising all study related procedures and finalizing the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All patients gave informed consent and the local ethics committee of the Medical University of Vienna approved of the study (1539/2020).
Consent for publication
Not applicable.
Competing interests
All authors report no conflict of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kautzky, A., Nopp, S., Gattinger, D. et al. Sex differences of post-Covid patients undergoing outpatient pulmonary rehabilitation. Biol Sex Differ 15, 36 (2024). https://doi.org/10.1186/s13293-024-00609-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13293-024-00609-z